By Sophia Deschler RN, BSN, RN | BSN
Updated on November 3, 2023
Published on August 21, 2023
Fact Checked

Get latest news, updates, and trends on mental well-being
We’ve all dealt with stress. It’s a normal part of life, whether it’s the subtle pressure of rushing to get to work on time or a traumatic event like losing a loved one. In a way, some stress can be a good thing. But you don’t want it to get out of hand.
Three-quarters of American adults have experienced stress-related health issues.1 Anxiety, depression, and other mental health issues are becoming increasingly common,2 and these conditions can really get in the way of your daily life.
Stress, anxiety, and depression are interrelated. They feed into one another, meaning when one gets worse, the others do too. Their symptoms are similar, and when you’re experiencing one, you may also experience the other.
So, with how common chronic stress and mental health conditions are, it is incredibly important to understand the connection between them.
This article covers everything you need to know about how anxiety, stress, and depression are interrelated and how to manage this triad so they don’t affect your daily life.
To understand how these three conditions are closely related, you must first understand each condition and their similarities.
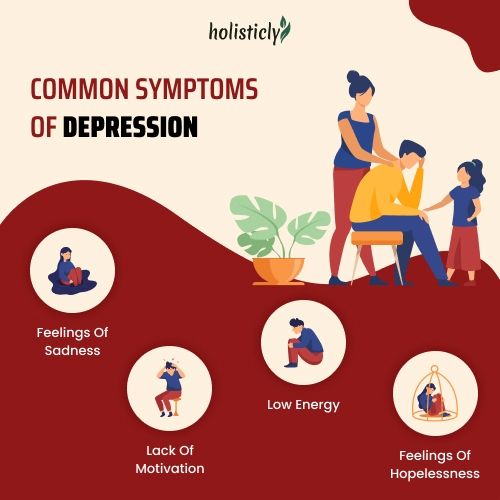
Depression is a mental illness that causes irregular moods and persistent feelings of sadness. This mental health condition can be related to a variety of different circumstances, such as a genetic tendency and/or environmental factors.3
There are various depression disorders, including:
Common symptoms of depression include:
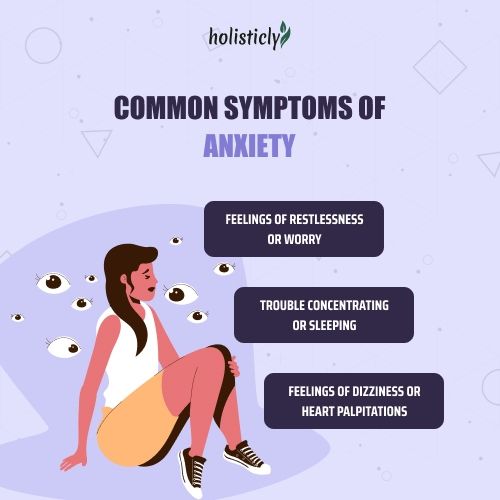
Anxiety is a feeling of worry or fear.4
Anxiety may be a short-term experience caused by a specific stressor, or if you have an anxiety disorder, you may experience it even in a normal situation.
Sometimes anxiety is caused by other conditions such as panic disorders, phobias, and post-traumatic stress disorder (PTSD).
Common symptoms of anxiety include:
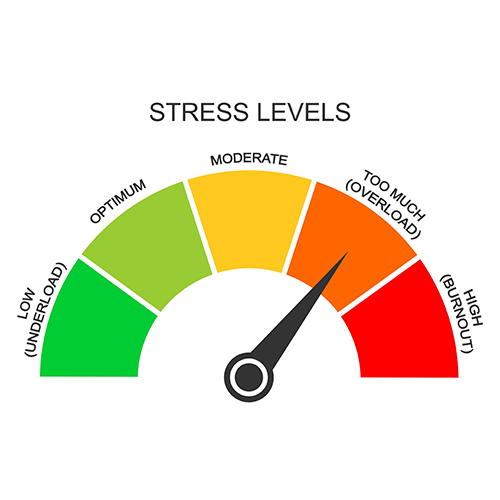
Stress is a state of worry.5 It prompts us to make certain adjustments for safety – think running away from a lion chasing you.
Stress is typically triggered by an outside event, such as running late for work or feeling unsafe. For this reason, it is considered a healthy biological reaction.
However, when stress goes unmanaged, it can lead to various health conditions and hinder quality of life.
Stress, anxiety, and depression have many similarities. All three can get in the way of everyday life when left untreated. Sometimes, poorly managed stress can lead to anxiety and depression or worsen these conditions.
It can be hard to distinguish between anxiety and stress since both have similar symptoms. The main difference is that anxiety is a reaction to stress.
Stress is more often a normal reaction to life events but chronic stress can definitely be hindering. Chronic stress can lead to anxiety and depression.
The Depression Anxiety Stress Scale (DASS) is an assessment tool6 used by doctors to measure a person’s severity of experiencing anxiety, depression, and stress.
When this exam is administered, you will answer 42 questions on a 4-point scale.
Higher scores mean a higher severity of depression, anxiety, or stress. The test usually takes about 10 to 20 minutes to complete. This test gives doctors an idea of how severely their patients are experiencing these emotions.
Doctors use this test in combination with other tests and assessments to help diagnose and treat patients with mental health challenges.
The connection between stress and depression is “bidirectional,” meaning one causes the other and can worsen the other.
Chronic stress can change your brain7 in ways that worsen symptoms of depression and make the condition worse.
There are a few main ways that stress and depression fuel each other8:
It’s no surprise that stress and anxiety are linked, given that the two are so similar they are often mistaken for one another. Anxiety is usually a result of stress.10
For example, if you struggle with chronic stress, you may start to feel anxious even in situations that shouldn’t be anxiety-inducing because you’ve been holding on to unresolved stress.
When you feel stressed, your body releases certain hormones to help increase your energy and biologically adapt your body to fend for itself. When stress is unmanaged, these hormones can be released inappropriately, causing you to live in a “fight-or-flight” state.
You can become worried and preoccupied with your stress, increasing anxiety levels even further. Additionally, chronic stress often leads to unhealthy lifestyle habits like binge drinking, eating unhealthy foods, and self-isolation, which worsen mental health issues.
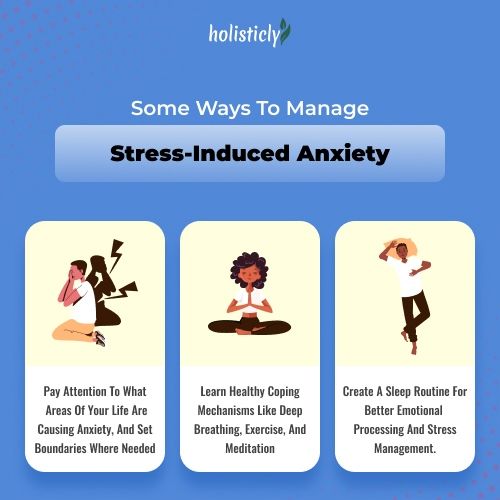
Some ways to manage stress-induced anxiety include:
All three of these conditions play into each other. Many studies have pointed to the connection between chronic stress and depression and anxiety.
There is also a subtype of depression called “anxious depression,” which is more severely influenced by chronic stress.7
Chronic stress has many effects on the brain, which can worsen and contribute to mental health issues like anxiety and depression.
It is important to find healthy coping strategies to manage stress, anxiety, and depression to prevent these issues from worsening so you can live a happy life.
Some helpful coping strategies for the overlapping triad of anxiety, stress, and depression include:
Quickly taking action can help prevent anxiety, depression, and stress from getting out of control.
Some lifestyle practices to help prevent the triad of anxiety, depression, and stress include:

Depression, stress, and anxiety all feed into each other. Chronic stress is incredibly common in our “go, go, go” society. It requires conscious effort to avoid chronic stress in your life, but these steps are essential to feeling your best.
When stress levels get out of hand, it can lead to various health issues, including depression and anxiety. When you take steps to overcome and prevent these conditions, you will notice positive changes in your life and realize that it is entirely worth the effort.